Anxiety and the Microbiome
Exploring the science around a commonly observed relationship
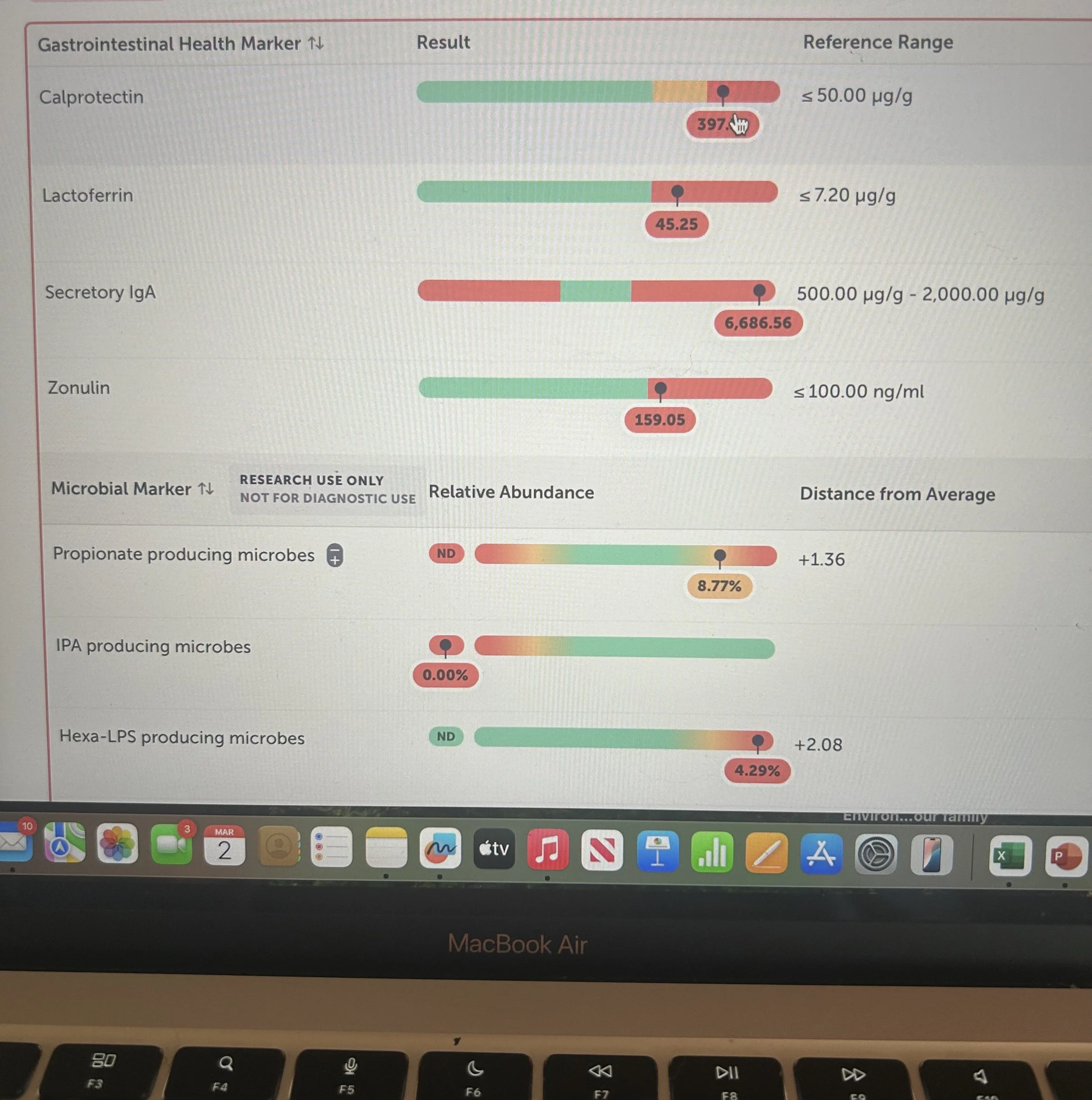
Interpreting many hundreds of microbiome test results I notice some very common threads connecting test results and mood behaviours, notably Anxiety.
Although observational data, I thought it worthy to explore and connect for you the science around my observations.
Scientific investigation of the gut–anxiety connection reveals significant associations between the composition of your gut microbiome and your psychological state.
In today’s fast-paced, on the go world, it’s no surprise that more and more people are struggling to feel relaxed or even get a good night’s sleep.
Between chronic stress, screen overload, and unresolved emotions, many are living in a near-constant state of nervous system dysregulation, often without realizing that it’s a manifestation of either anxiety, poor sleep or an unhealthy biome.
And it shows up in ways that sadly we’ve normalized:
✅ Racing thoughts
✅ Exhaustion despite sleep
✅ Irritability and overwhelm
✅ Sleep struggles
✅ Anxiety that seems to come from nowhere.
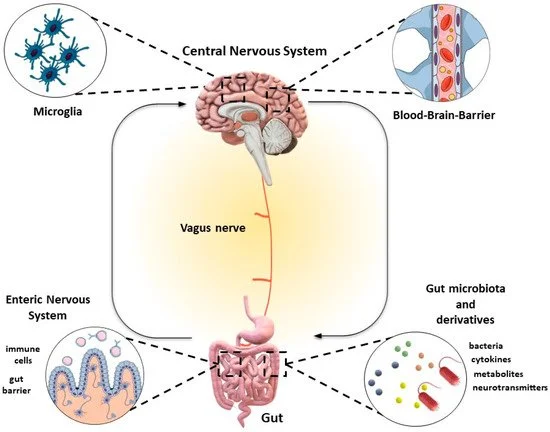
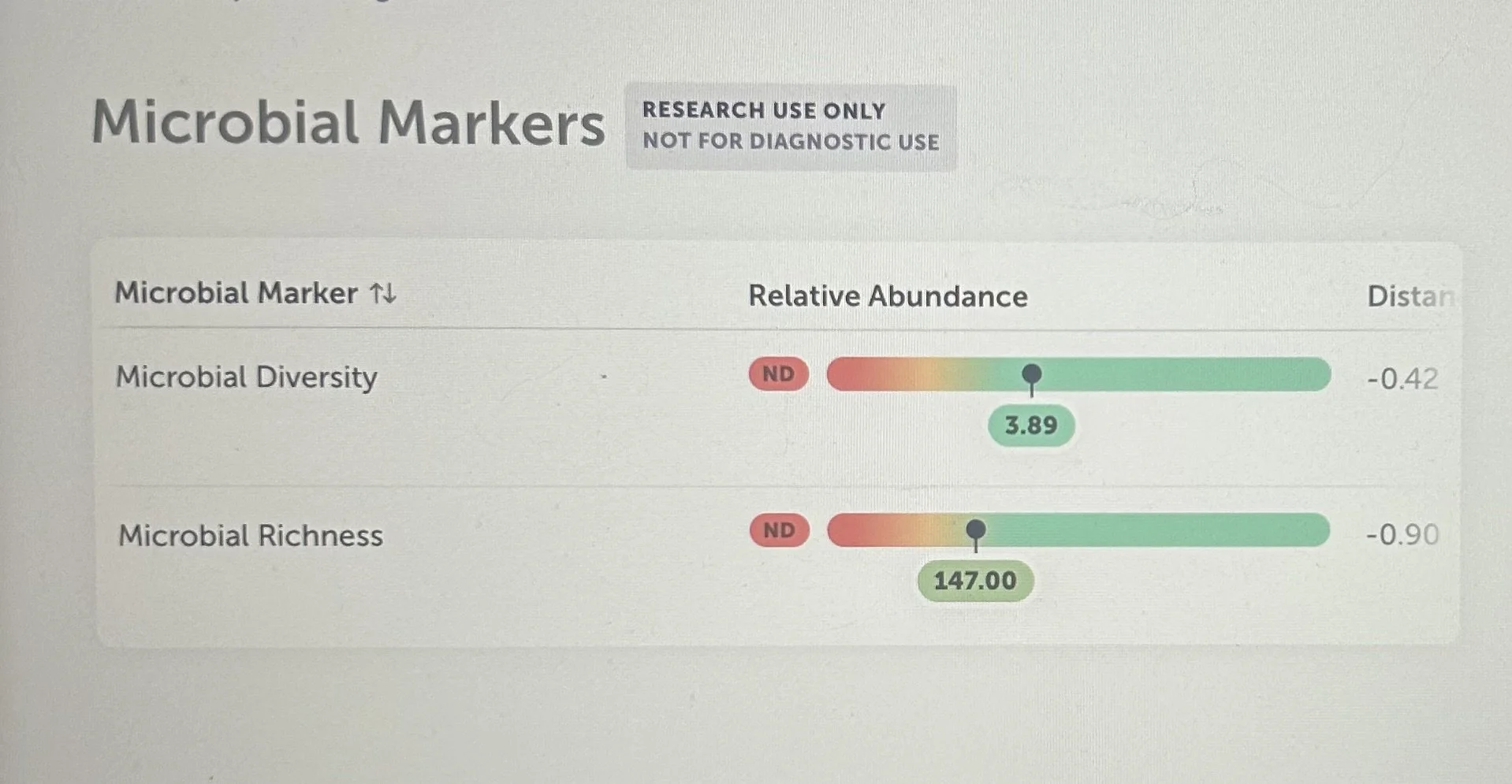
In clinical practice while working with Microbiome testing, I see constant recurring patterns characterised by a reduction in microbial diversity, a decrease in the number of microbes and alterations in community composition.
These microbiome shifts often correlate with changes in mood and anxiety states, suggesting a critical role of gut microbiota in the regulation of neuropsychiatric and emotional health.
Understanding these connections between genes and metabolism may explain how the gut–brain link affects anxiety disorders.
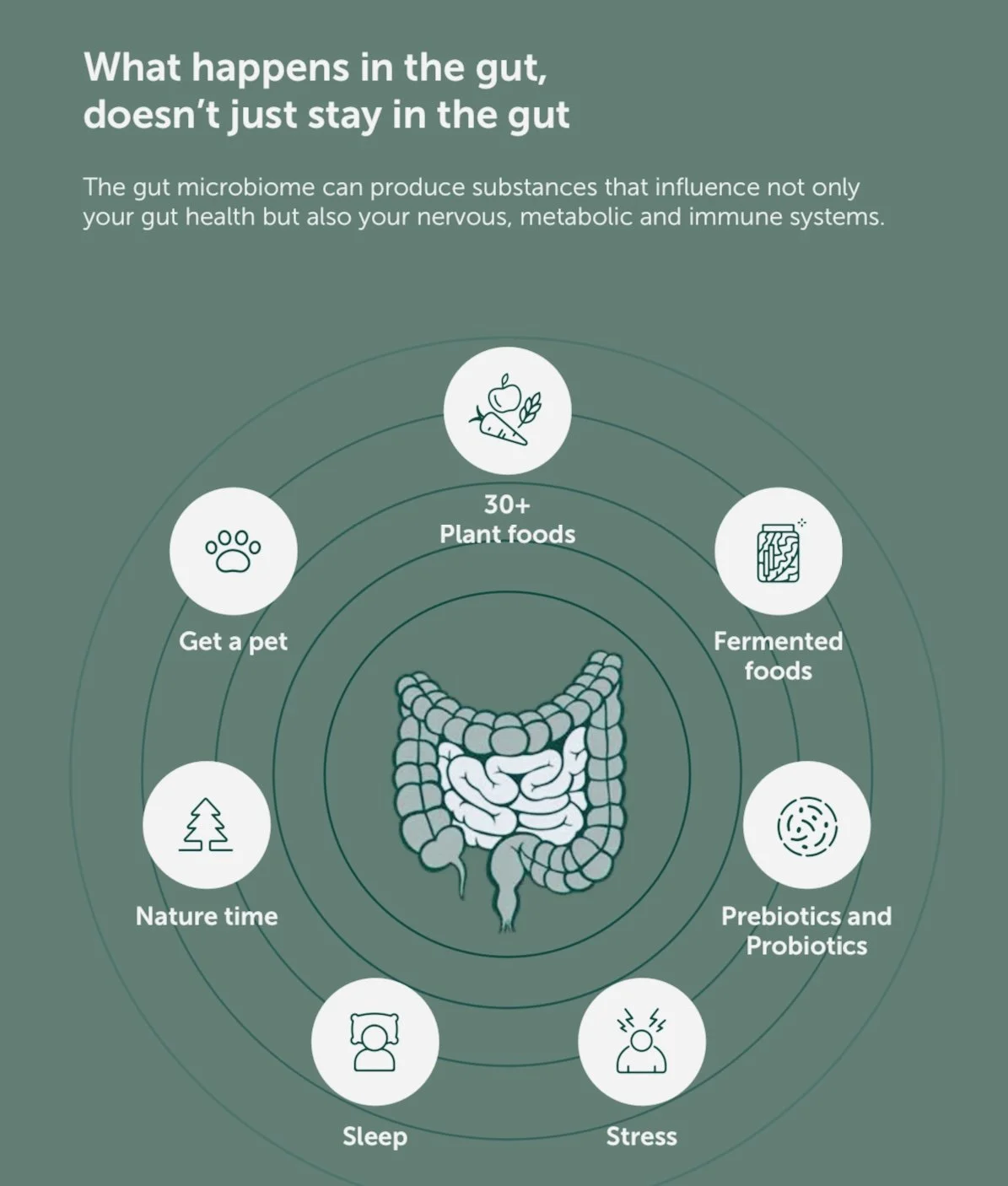
Your gut and brain are in constant conversation — this is known as the gut-brain axis. The trillions of bacteria living in your digestive tract (your microbiome) send signals that can shape how you feel, think, and even respond to stress. A healthy and diverse microbiome doesn’t just support digestion — it helps protect your mental wellbeing.
Research shows us that people with richer, more diverse gut microbiomes tend to have greater resilience to stress and anxiety, while those with lower bacterial diversity may be more vulnerable to mood disorders.
Gut Microbiome Richness: A Foundation for Stability and Calm
In a landmark French study (Tap et al., Environmental Microbiology, 2015), researchers found that:
People with higher microbiome richness — meaning more types of beneficial bacteria — had more stable gut ecosystems, even when their diet changed.
These rich microbiomes produced more short-chain fatty acids (SCFAs) such as butyrate, caproate and valerate, known to support gut lining integrity, immune balance, and brain health.
A diverse microbiome was linked to higher levels of helpful bacterial groups like Prevotella and Coprococcus, Lactobacilli, Bifidobacterium, all known for producing anti-inflammatory and neuroprotective compounds.
In a landmark study published in *Frontiers in Gastroenterology related Frontiers review (2022) by Carabotti, M., Scirocco, A., Maselli, M. A., & Severi, C.
“Gut microbiota in anxiety and depression: Pathogenesis and therapeutic perspectives”
In this mechanistic review the authors described how microbiome alterations (including reduced diversity and loss of beneficial metabolite producers) can influence neuroimmune, metabolic, and neurochemical pathways linked to anxiety and mood disorders
Key Takeaway: A rich microbiome helps your gut stay balanced during life’s dietary or emotional stressors — protecting both digestion and mood.
Gut Health and Anxiety: What Science Reveals
A 2025 review (Butler et al., Current Psychiatry Reports) highlighted that people with generalised anxiety disorder (GAD) often show:
Reduced bacterial diversity
Lower levels of beneficial bacteria like Eubacterium, Faecalibacterium, and Coprococcus
Higher levels of inflammatory species like Fusobacterium and Escherichia-Shigella
These shifts can alter the production of calming neurotransmitters, impact the immune system, and affect stress hormone regulation via the HPA axis (the Hypothalamus, Pituitary axis, a crucial stress regulating connection).
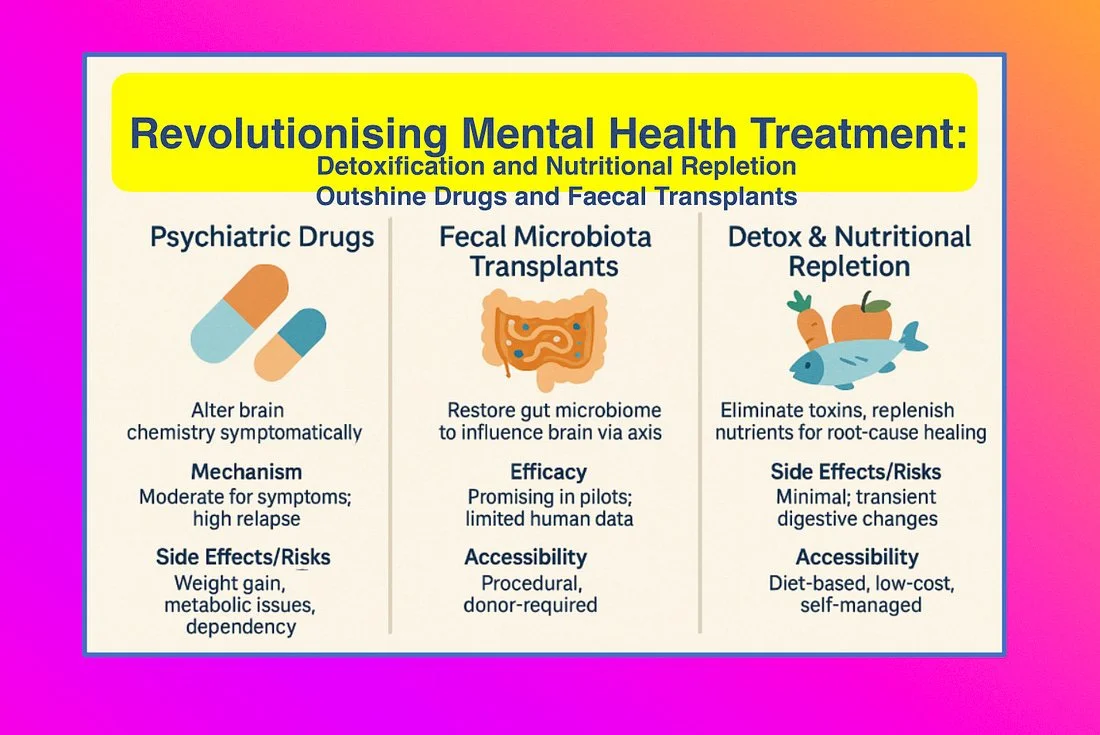
In short, imbalanced gut bacteria may fuel anxiety, while restoring balance may help calm it.
The Mechanisms: How a Healthy Gut Supports a Calm Mind
Your gut bacteria communicate with your brain through several pathways:
🧬 Short-chain fatty acids (SCFAs): Produced when gut bacteria ferment dietary fibre; they support a healthy gut barrier and modulate inflammation, indirectly improving mood.
💫 Tryptophan metabolism: Healthy bacteria help convert tryptophan into serotonin (the “feel-good” neurotransmitter).
🧠GABA is produced and consumed by gut microbes. GABA is a calming and protective neurotransmitter.
⚡ Vagus nerve signalling: Gut microbes send calming signals directly to the brain through this major nerve pathway.
🧠 Brain plasticity: Some bacterial metabolites promote the production of BDNF, a brain growth factor linked to resilience against anxiety and depression.
Mind Your Stress
Chronic stress alters the gut microbiome.
Incorporating mindfulness, breathwork, and regular movement can reduce this disruption — helping your microbes and your mind thrive together.
Natures prescription is free and available and suitable to all.
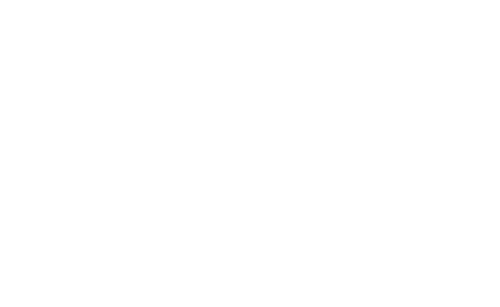
Building a Rich and Resilient Microbiome Naturally
These studies point to the same simple truths: feed your microbes well, and they’ll take care of you and support healthy mood and help you maintain healthy weight.
🥦 Increase Microbial Richness
Eat diverse plant foods — aim for 30+ different fruits, vegetables, herbs, and legumes weekly.
Include fermented foods (yogurt, kefir, kimchi, sauerkraut) that introduce live beneficial bacteria.
Choose whole, fibre-rich foods such as oats, lentils, and leafy greens to fuel beneficial species like Faecalibacterium and Coprococcus.
Test for Gluten and Dairy sensitivity suggested.
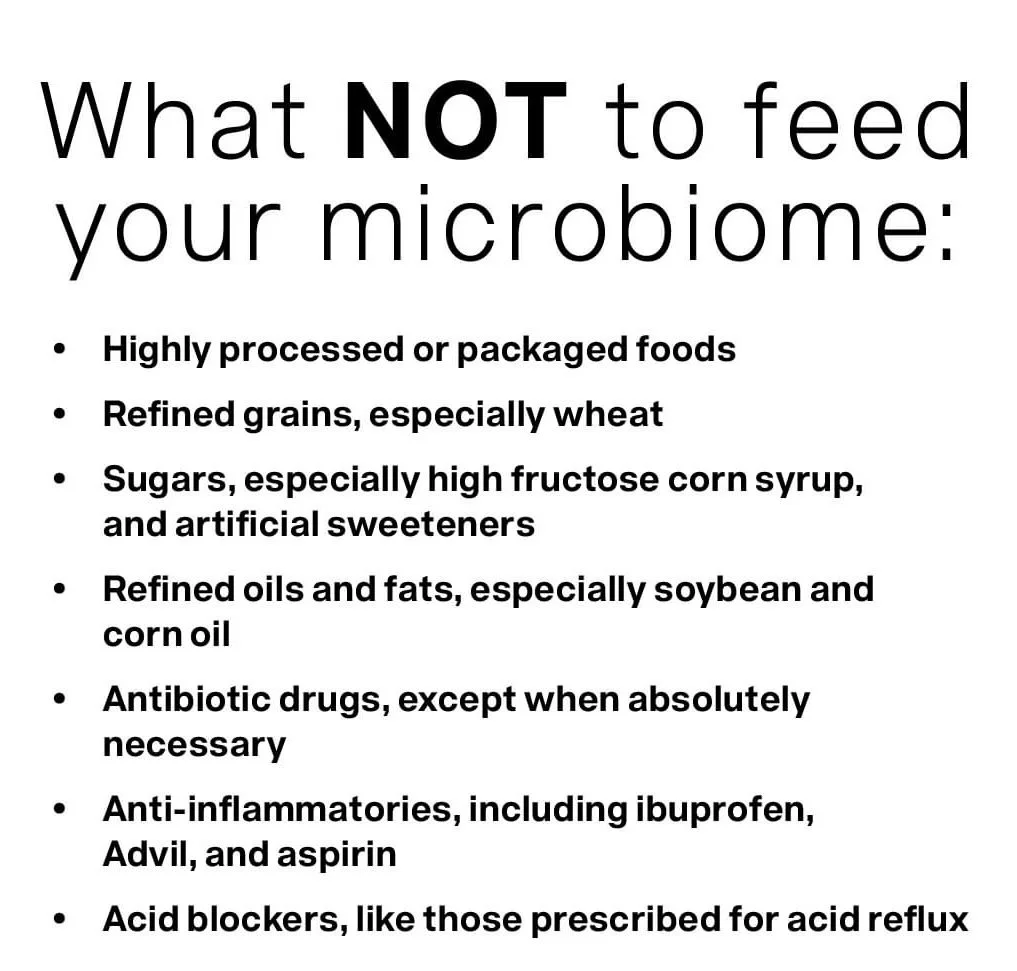
Limit ultra-processed foods, sugar, and alcohol, which deplete microbial diversity.
🌾 Focus on Fibre
The Tap et al. study showed that higher dietary fibre intake (40g/day) increased microbial activity, enriched beneficial metabolic pathways, and reduced gut inflammation.
Even modest increases in fibre (from fruits, legumes, and whole grains) can boost microbiome richness and mood stability.
Fibre is important HOWEVER, not all fibres are equal.
I use several different functional fibres in clinic depending on your microbial results.
For example, if I use high Resistant Starch foods + functional fibres with a patient who has tested as high Methane producing bacteria, it will make their symptoms a lot worse.
I advocate TEST don’t GUESS when balancing your biome.
The great news is that your biome has the capacity to shift in composition and behaviour after just a few weeks.
My Key Takeaways
Rich gut microbiomes offer more preventative health stability. Test don’t guess is an excellent strategy.
A diverse gut broadly and specifically resists stress
Low diversity is often seen in anxiety disorders and rebuilding diversity reduces anxiety risk.
Fibre fuels beneficial bacteria aim for 30–40g/day from varied plant foods however understand which is appropriate for you.
Gut bacteria can influence neurotransmitters “happy chemicals”.
Feeding your gut can help regulate mood.
Short Chain Fatty Acids (SCFA’s) like butyrate, caproate, valerate support brain health and are produced through fibre fermentation by the most beneficial microbes
A Co-Biome microbiome report is a test everyone should get for personalized health. Many studies show clear links between gut microbes and anxiety, depression and neurognitive disorders.
References
Butler M.I. et al. (2025). The Gut Microbiome in Anxiety Disorders. Current Psychiatry Reports, 27(347–361). https://doi.org/10.1007/s11920-025-01604-w
Tap J. et al. (2015). Gut Microbiota Richness Promotes Its Stability upon Increased Dietary Fibre Intake in Healthy Adults. Environmental Microbiology, 17(12), 4954–4964. https://doi.org/10.1111/1462-2920.13006
Kang, D.-W., Ilhan, Z. E., Isern, N. G., Hoyt, D. W., & Hsiao, E. Y. et al. (2021). Perturbations in Gut Microbiota Composition in Psychiatric Disorders: A Systematic Review and Meta-analysis. JAMA Psychiatry.
Summary: Large meta-analysis (59 case-control studies) showing transdiagnostic gut-microbiota perturbations in psychiatric disorders, with depletion of some anti-inflammatory/ butyrate-producing taxa and enrichment of pro-inflammatory bacteria. JAMA NetworkMcGuinness, A. J., Davis, E. L., & Simpson, E. (2020). The gut microbiota in anxiety and depression — a systematic review. Clinical Psychology Review / related systematic review (2020).
Summary: Systematic review of human studies reporting microbiome composition differences in anxiety/depression cohorts; several studies report lower α-diversity in anxious/depressed participants, though results vary by cohort and method. ScienceDirect+1Gao, M., Wang, J., Liu, P., Tu, H., Zhang, R., Zhang, Y., Sun, N., & Zhang, K. (2023). Gut microbiota composition in depressive disorder: a systematic review, meta-analysis, and meta-regression. Translational Psychiatry (Nature Group).
Summary: Recent systematic review/meta-analysis finding compositional shifts (loss of SCFA/butyrate producers, altered taxa) in depression; notes heterogeneity across studies and mixed results for alpha-diversity metrics. NatureCarabotti, M., Scirocco, A., Maselli, M. A., & Severi, C. (2022). Gut microbiota in anxiety and depression: Pathogenesis and therapeutic perspectives. *Frontiers in Gastroenterology / related Frontiers review (2022).
Summary: Mechanistic review describing how microbiome alterations (including reduced diversity and loss of beneficial metabolite producers) can influence neuroimmune, metabolic, and neurochemical pathways linked to anxiety and mood disorders — and discusses microbiome-targeted interventions. Frontiers